TULSA-PRO Prostate Treatment
Transurethral Ultrasound Ablation for Prostate Cancer and BPH
Broader than Focal, Less than Total
TULSA-PRO is a customizable, predictable, and incision-free procedure that allows the doctor to tailor the ablation to each patient.
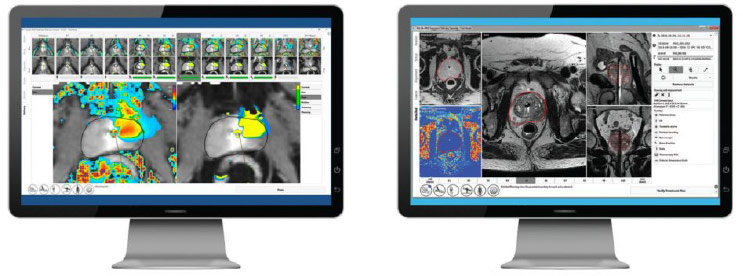
Real-Time Imaging
Directional Thermal Ultrasound
Closed-Loop Temperature Feedback
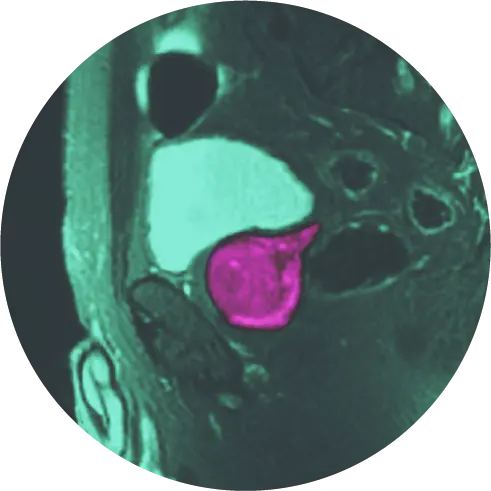
Transurethral ultrasound ablation (TULSA-PRO) can more easily cover a wider area than laser focal therapy (LFT) / focal laser ablation (FLA). For patients who have a relatively larger cancer, or somewhat diffuse cancer within the prostate, TULSA-PRO can cover almost the entire prostate gland in many patients.
Advantages of TULSA-PRO
Decreased Risk of Side Effects
TULSA-PRO has a decreased risk of erectile and urinary side effects compared to whole gland therapy.[1]
Same-Day Outpatient Procedure
TULSA-PRO is performed in a single session that takes a few hours.
Keep Your Options Open
If you are in need of future prostate care, you may either have a repeat TULSA procedure, or choose any other type of prostate therapy to address your prostate needs.[2]
Advanced Image Guidance
Directional thermal ultrasound and MR imaging with active heat monitoring.
Customizable Treatment Plans
TULSA-PRO is customizable and personalized based on your situation and goals.
Shared Decision Making
Before your TULSA procedure, you will decide with your physician on a treatment plan.
1 Hatiboglu G, Popeneciu V, Bonekamp D, Burtnyk M, Staruch R, Distler F, Radtke JP, Motsch J, Schlemmer HP, Pahernik S and Nyarangi-Dix J (2021) Single-Center Evaluation of Treatment Success Using Two Different Protocols for MRI–Guided Transurethral Ultrasound Ablation of Localized Prostate Cancer. Front. Oncol. 11:782546. doi: 10.3389/fonc.2021.782546 | 2 Nair, S.M., Stern, N., Dewar, M. et al. (2020). Salvage open radical prostatectomy for recurrent prostate cancer following MRI-guided transurethral ultrasound ablation (TULSA) of the prostate: Feasibility and efficacy. Scandinavian Journal of Urology, 54(3), 215-219. doi: 10.1080/21681805.2020.1752795
How it Works
TULSA-Pro for Prostate Cancer
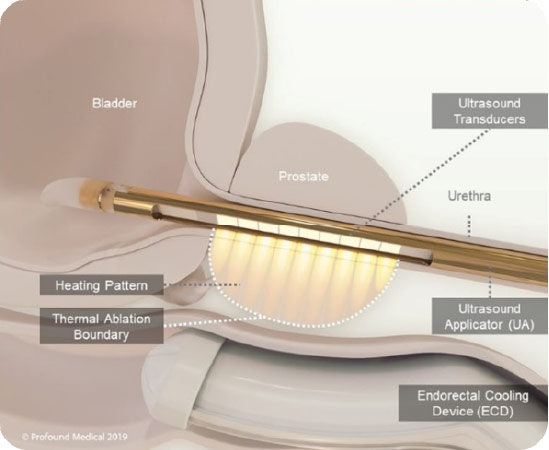
The Transurethral Ultrasound Ablation (TULSA) Procedure is a minimally invasive procedure that uses directional ultrasound to produce very high temperatures to ablate (destroy) targeted prostate tissue. There are no incisions or radiation.
The procedure is performed in a Magnetic Resonance Imaging (MRI) suite and uses the TULSA-PRO® system to ablate prostate tissue from the ‘inside-out’. The procedure combines real-time MRI with robotically-driven, directional thermal ultrasound to deliver predictable, physician-prescribed ablation of whole gland or partial prostate tissue.
TULSA-Pro for BPH
BPH is not prostate cancer, but TULSA-PRO has proven to successfully treat BPH with no incisions, radiation, and with a lower risk of side effects.
TULSA-PRO is an effective option for men with BPH as it destroys enlarged prostate tissue while avoiding damaging vital structures. The procedure is completed in one treatment session and performed under general anesthesia.
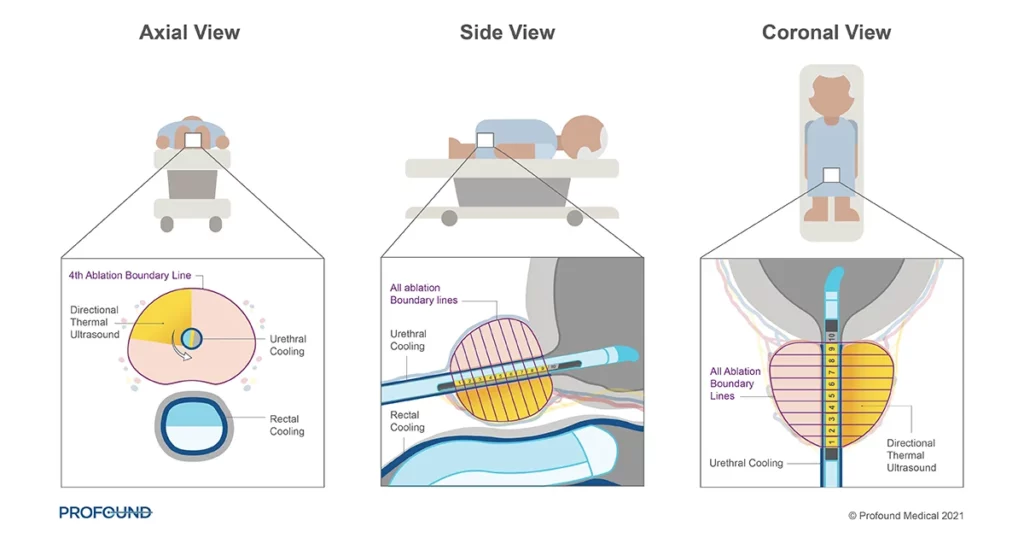
Individualized Elements
After the placement of the device and initial MRI scanning, the physician enters a treatment plan. The TULSA-PRO system then individually controls ten separate elements, allowing for broad tissue destruction while fine tuning each treatment area. This is all performed under the watchful eye of the physician who can make adjustments as appropriate.
The device actively protects the urethra and rectum with cooling during treatment. This cooling maintains a safe temperature for these critical structures to prevent damage.
Performing the TULSA Procedure
The TULSA procedure (TULSA-PRO) ablates prostate tissue from the inside out. A device enters the urethra which delivers thermal ultrasound energy outwards from the urethra to the prostate while under real-time MRI guidance.
This approach avoids the need for surgical incisions to reach the prostate. A cooling mechanism helps protect the urethra from the ultrasound energy. The thermal ultrasound energy is delivered in a sweeping motion (visualize a clock hand sweeping), which enables the physician to ablate a wider area.
How Dr. Karamanian, prostate program medical director at HALO Dx, performs the TULSA procedure
Controlled and Predictable
TULSA-PRO produces real-time temperature maps, enabling the physician to see the increasing temperature of the prostate tissue and surrounding structures every 5-7 seconds during treatment. This visibility allows the physician to actively monitor tissue heating.
The physician can make adjustments to the plan if necessary, enabling the procedure to be very controlled and predictable.
Frequently Asked Questions
Can the TULSA procedure (TULSA-PRO) perform partial and whole gland ablation?
Our physicians can customize the procedure to ablate a specific area of the prostate or almost the entire prostate, depending on your needs and functional outcome goals.
Can the TULSA Procedure (TULSA-PRO) treat a median lobe (growth of the prostate into the bladder)?
Generally, yes. The physician can customize the procedure to ablate specific areas of the prostate based on the patient’s needs.
What are the side effects?
As with many procedures, there are side effects associated with the TULSA procedure. The most common side effects include pain/discomfort in the procedure area, blood in urine, urinary tract infection, urinary incontinence, and erectile dysfunction. According to the TACT: TULSA® Ablation Clinical Trial conducted by Profound Medical (the makers of TULSA), the study found patients had a 2.6% urinary incontinence risk and 25% erectile dysfunction risk.
Who qualifies for TULSA-PRO?
Whether a patient qualifies for the TULSA procedure will be determined by the treating physician on a case by case basis. In general, patients should have low to intermediate risk disease which is confined to the prostate. Generally, the patient should have a PSA of less than 20. If a patient has significant calcifications within the prostate (as determined by a CT scan), then they are not a candidate for TULSA, because the calcifications will block sound waves. Patients should be relatively healthy and able to undergo general anesthesia. Contact us if you would like more information.