Laser Focal Therapy for Prostate Cancer
Laser Focal Therapy for Prostate Cancer
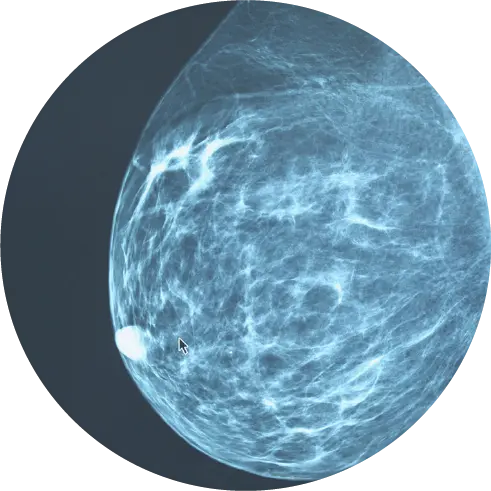
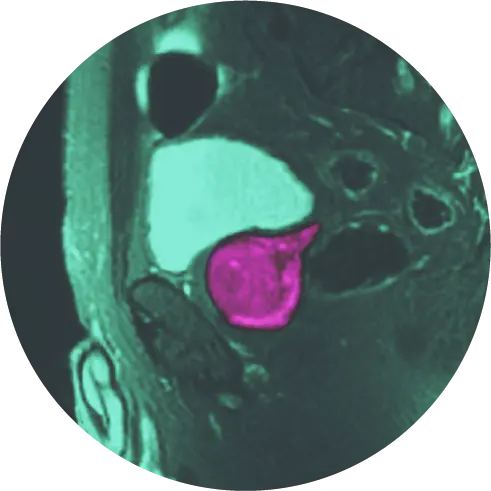
At HALO Diagnostics, we use Laser Focal Therapy (focal laser ablation) for the treatment of low-to-intermediate prostate cancer and to help improve the symptoms associated with benign prostatic hyperplasia (BPH). This procedure involves placing the patient inside the MRI scanner and displaying MRI images and thermal maps on a computer screen. A thin laser fiber is guided to the tumor and laser energy is applied to kill the cancer cells. The temperature and the extent of the ablation zone are constantly monitored with MRI imaging, allowing HALO Dx clinicians to determine if all visible tumors have been destroyed.
Advantages of Laser Focal Therapy (Focal Laser Ablation) for Prostate Cancer
- Minimally invasive, ambulatory outpatient procedure (usually lasts 4 hours and patient can go home after).
- Rapid recovery: most patients can return to work the next day.*
- No general anesthesia required.
- Vast majority of men have improved urination after the procedure.*
- Lower risk of side effects such as urinary incontinence, impotence and decreased bowel function compared to surgery or radiation therapy.
- Better accuracy compared with other focal approaches, e.g. High-Intensity Focused Ultrasound (HIFU).
- Unlike other treatments, focal laser therapy does not limit the option to treat with radiation therapy or surgery if needed later.
Traditional Approaches Like Radical Prostatectomy (RP) Have Severe Side Effects
- 50% risk of erectile dysfunction (impotence)
- 25% risk or urinary incontinence
- Dry orgasm
- 20-40% cancer recurrence within 10 years, 30-50% cancer recurrence during patient’s lifetime
What is Laser Focal Therapy?
In 2010, the team of Bernadette Greenwood, Chief Research Officer at Halo Diagnostics, and Roger McNichols, PhD, developed the system to perform Laser Focal Therapy. The first case in the world was performed by the HALO Diagnostics team of Dr. John Feller, Ms. Greenwood, and Dr. McNichols in 2010.
HALO Diagnostics released interim 10-year results from its Phase II 20-year clinical trial for prostate laser focal therapy in patients with localized prostate cancer. Over 170 men, 45-years or older diagnosed with low-to-intermediate risk or recurrent prostate cancer, volunteered to participate in the study. The results are impressive: less than 1% infection, less than 1% erectile dysfunction and less than 1% incontinence – compared to conventional whole gland prostatectomy which has a risk of up to 50% erectile dysfunction and 25% urinary incontinence. These results, along with a 100% prostate cancer-specific survival rate, are an encouraging development for men looking for a prostate cancer therapy option with a lower risk of side effects.
Attacking Cancer with Laser Precision
Laser focal therapy can be advantageous to other forms of treatment for prostate cancer, as it can result in a higher quality of life for the patient. This is largely due to the ability to only target cancerous cells, leaving healthy cells intact. Laser focal therapy has the most precise temporal and spatial tools, increasing the level of detail and reducing the chance of error. The laser is able to operate at levels down to 0.5 millimeters, which allows the laser to have more precise focus on the targeted area of the prostate and not disrupt the surrounding healthy tissue. In addition, an MR thermometer and safety controls are used during the therapy for a smooth operation with real-time feedback. Other energy sources used in different forms of prostate operations are not compatible with MRIs, making those operations less safe due to a lack of real-time feedback.
*Results may vary
How Does Laser Focal Therapy Compare to Other Focal Methods?
In comparison to another popular focal treatment methods, like high-intensity focused ultrasound (HIFU), laser focal therapy is not limited to only small glands and has demonstrated much higher levels of accuracy with lower risk of side effects such as, erectile dysfunction.
High intensity focused ultrasound (HIFU) uses ultrasound instead of laser to heat the tissue. To obtain the ablation diameter (area of cancerous tissue being killed) of the laser used in our approach, HIFU would require >20 overlapping ablations. What if the patient moves a little and the device misses a spot? When treating cancer, it’s important to get all of it. The vast majority of HIFU centers use ultrasound guidance (instead of MRI), losing the precision of MRI and the important real-time information that MRI thermometry (temperature measurement) provides in protecting vital structures. Studies show significant urinary and sexual problems after HIFU because important tissues and nerves can be damaged during the procedure.
Laser focal therapy boasts many benefits for patients compared to other treatment methods for prostate cancer. No general anesthesia is required for the therapy, and patients are able to return to work as early as the day after the operation. Additionally, laser focal therapy carries lower risk of side effects compared to other treatment methods such as, impotence, and urinary incontinence. Laser focal therapy also does not rule out the exploration of further treatment options such as surgery or radiation therapy if needed later.
When deciding which type of prostate cancer treatment to choose, it is important to consider how each treatment differs and how this may impact the treatment results.
*Results may vary
Laser Focal Therapy: What to Expect
Here When You Need Us Most
You will receive both email and phone contact information for our medical team so that you can always reach us. In addition, we conduct a pre-operative consultation prior to the procedure, we meet the day of the procedure, and will see you frequently in follow-up.
Before Your Procedure
Our team will have collected and reviewed your medical records to evaluate you for inclusion and suitability. Our surgical team will have discussed your case during Tumor Board and conducted a surgical plan based on size, number, shape and location of ablation areas. Prior to the procedure, we will review the Informed Consent Document with you to ensure you understand every aspect of the procedure. We will discuss the risk, benefits, and paperwork of the procedure.
Day of Your Procedure
The day of the procedure, our nurse will place an intravenous catheter (IV) in your arm so that she/he can administer IV antibiotics, pain medications and fluids (to maintain hydration). Should other medications be necessary, they will be administered through this IV as well.
You may have a urinary catheter placed so that we can provide cooled urethral saline through Continuous Bladder Irrigation (CBI) protection. This catheter remains in place depending on the size, shape, and location of treatment. Our urologist will perform the insertion and removal.
Patients are positioned on their stomach on the MRI table for the procedure. A small rectal probe (the diameter of an index finger in width) covered in numbing jelly to allow access to the prostate. We use the transrectal route for laser fiber placement. This is minimally invasive (compared to thermocouples and transperineal needles), with fewer complications and less recurrence. Technical errors due to misregistration are also less frequent with transrectal fiber placement under MRI guidance.
During the procedure, we will use real-time MRI to visualize the target, guide placement of the laser fiber, and ablate (destroy) cancer cells or for either cancer or BPH (an overgrown transitional zone) while protecting healthy tissue with “safety markers” that are positioned at the urethra and neurovascular bundle. This helps monitor sensitive structures to decrease risk of damage to urinary and sexual function.
After Your Procedure
Patients will return home or to their hotel room after at least two hours in the recovery room that same day. They must be accompanied by a family member or care giver as driving is not permitted.
We see each patient again according to our rigorous follow-up protocol. This includes follow-up imaging, biopsy and PSA monitoring.

Detailed Procedure Overview
- An MRI before the procedure confirms the location and boundaries of the target area(s).
- A surgical device (DynaTRIM) is calibrated to the MRI images, and the parameters are adjusted to an appropriate three-dimensional approach to target the tumor(s).
- The thin 1.85mm cooling tube, also called a cannula, and an FDA cleared laser fiber is then placed into the target through the inner channel of the surgical device (DynaTRIM) under MRI guidance.
- Continuous bladder irrigation may be performed to help protect the external urethral sphincter.
- The laser is then applied at low power “test dose” to confirm appropriate location with the heat from the laser being monitored with real time MRI thermometry in two separate planes. Only after this final confirmation, the team will increase the laser to treatment level power, monitor the tissue being ablated and make appropriate adjustments to contour the ablation zone.
- The laser fiber is usually then repositioned multiple times to provide overlapping ablations. Because we believe in obtaining wide margins, we will usually perform many overlapping ablations.
- At the end of the treatment, we evaluate the result with contrast enhanced MR imaging.
Do I Qualify for Laser Focal Therapy?
We’re here to answer all of your questions. Please fill out the below form and one of our specialized team members will contact you with further information and next steps.