Mammograms are an essential part of routine preventive healthcare for women, yet many women put off their screening because they are worried it will be painful and time-consuming.
Let’s face it. Getting a mammogram can be a little daunting. However, a mammogram is an important screening procedure that allows doctors to screen for breast cancer and detect it at an early stage.
In this article, we’ll help you understand what you can expect during your mammogram and answer some of the common questions that you may have about screening.
What Happens During a Mammogram?
Ahead of your mammogram appointment, you will be asked to refrain from wearing deodorant or powder products. Once you arrive for your appointment you will be taken to a private area where you will be given a gown and asked to remove your clothes from the waist up. Plan to wear a two-piece outfit that day for your convenience.
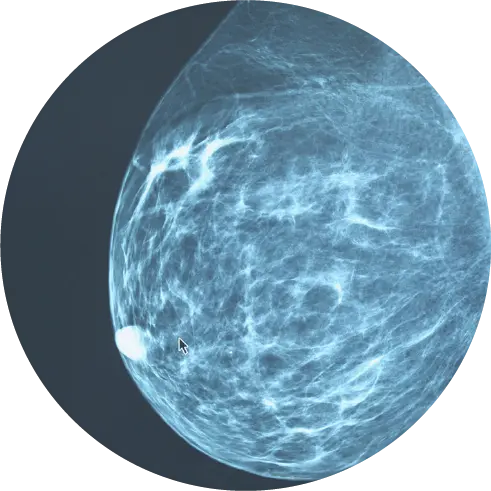
Once you are changed and you are comfortable, your mammo tech will guide you to the imaging suite. The trained technologist will position your breasts one at a time between two imaging plates. The upper plate will lower, compressing your breast for 10 to 15 seconds while the technologist takes each X-ray image. During this process, the technologist will ask you to hold your breath while they take the images.
Typically, two views of each breast are taken for a screening mammogram. However, more images may be needed if you have breast implants, dense breasts, or large breasts. The whole procedure takes only about 20 minutes.
Our centers only use 3D mammogram imaging which is the latest gold standard in imaging.
Is a Mammogram Painful?
A common myth about mammograms is that they are painful. The compression of your breast is necessary to get a clear image and may cause minor discomfort for 10 to 15 seconds, but the test itself is not painful.
To reduce discomfort, avoid scheduling your mammogram the week before your menstrual cycle as this is a time that your breasts may be more tender. Also, caffeine can increase breast tenderness, so skipping coffee the day before and the day of your appointment may be a good idea.
Be sure to let your technologist know if you experience pain during your screening, as they can make adjustments to increase your comfort. However, it’s important to keep in mind that compression is needed for clear images and any discomfort will only last for a few seconds.1
Does Family History Play a Role in the Screening?
Yes. If you have a family history of breast cancer, it’s essential to share that information with your doctor before getting a mammogram.
Women with close family members who have been diagnosed with breast cancer have a higher risk of developing the disease. Because of this, your doctor may ask you to get your first mammogram earlier than the recommended age of 40. For example, if your mother was diagnosed with breast cancer at the age of 42, you would be appropriate for screening 10 years prior to her diagnosis, based on societal guidelines and recommendations by your physician.
You should also let your provider know if you have experienced any symptoms or have had prior surgery or hormone use. With this information will help your doctor recommend a personalized screening plan that is best for you.2
How Long Does It Take to Learn Results?
Most people receive their routine mammogram results within two weeks. A radiologist usually reviews the images within 48 hours of your appointment and then sends their report to your doctor.
Your doctor then mails you the results, which can take another few days.
If the mammogram detects any abnormalities, your doctor or the radiologist will contact you sooner. It’s a good idea to check with your provider ahead of time to ask about their timetable.
Be sure to go over your mammogram results with your provider so that you fully understand the information.3
What Happens if My Results Are Abnormal?
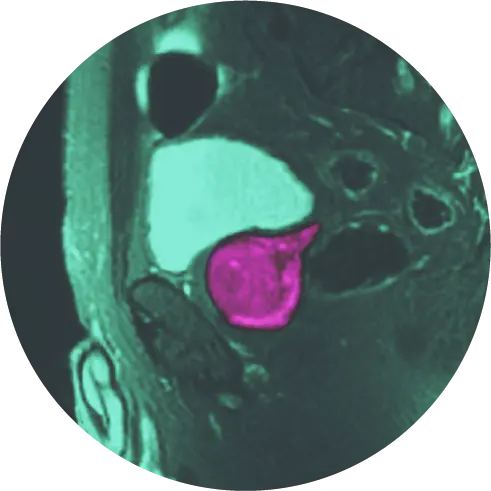
It is not at all unusual for a mammogram to indicate an abnormality in the breast tissue—especially with a first mammogram when there are no previous images to use for comparison.
In most cases, these suspicious findings are caused by dense breast tissue, benign cysts, or even an unclear mammogram image. In other words, most abnormalities are not cancer.
If your scan does indicate an abnormality, you may be called in for a diagnostic mammogram as a precautionary measure so that the radiologist can gain clarification on the image. In some situations, your doctor may recommend a breast ultrasound.4 It is important to note that 98% of abnormalities seen in these images are considered benign (not cancer), so there is no need to assume the worst.5
Debunking Some Mammogram Myths
Mammograms are proven diagnostic tools for breast cancer that lead to less aggressive treatment and better prognoses. Unfortunately, some myths persist that keep some women from making mammograms part of their routine healthcare. We’ve already addressed the myth concerning pain; here are some other common myths:
1. Myth: I don’t need a mammogram if I don’t have a family history and I’m not experiencing any symptoms.
Fact: More than 75 percent of women who have breast cancer have no family history of the disease. The American College of Radiology recommends yearly screening mammograms for all women over the age of 40.
According to the American Cancer Society, women with early-stage breast cancer have a five-year survival rate of 99 percent. For women with later-stage cancer, that rate is 27 percent.6
2. Myth: Mammograms have unsafe levels of radiation.
Fact: Mammograms use very low doses of radiation compared to X-rays. The benefits of this low dose far outweigh any possible risk.
Also, mammography is highly monitored and regulated by the FDA, the American College of Radiology, and the Mammography Quality and Standards Act.7
3. Myth: After a normal mammogram last year, I don’t need to have another one this year.
Fact: Having an annual mammogram increases the chances of detecting cancer when it is small and most easily treated.8
4. Myth: I need a doctor’s recommendation or prescription to have a mammogram.
Fact: You do not need a doctor’s referral to have a screening mammogram. All you need to do is make an appointment. Finally, there’s no need to feel afraid of this essential diagnostic tool. Rather, make it part of your routine healthcare, just as you do with your dental checkup and other forms of preventive care.
HALO Diagnostics is Here to Help
Are you ready to take control of your breast health? It’s as simple as setting up your first mammogram. If you have any further questions about getting a mammogram or would like to make an appointment, give us a call at (877) 225-2831 or reach out to us here.
References
- https://www.nationalbreastcancer.org/breast-cancer-faqs/are-mammograms-painful/
- https://www.breastcancer.org/risk/risk-factors/family-history
- https://www.medicalnewstoday.com/articles/how-long-does-a-mammogram-take
- https://www.mdanderson.org/publications/focused-on-health/FOH-first-mammogram.h16-1589835.html
- https://www.komen.org/breast-cancer/screening/mammography/mammogram-images/
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/breast-cancer/6-mammogram-myths
- https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/mammogram-basics.html
- https://www.mayoclinic.org/tests-procedures/mammogram/expert-answers/mammogram-guidelines/faq-20057759