Genetic changes that cause cancer can happen in several ways—and with several different outcomes. Learn how and why these mutations happen, what they mean for cancer risk, and what you can do once you know your risk.
What is a Genetic Mutation?
Genetic mutations are changes to your genes. Genes are found within the DNA, which in turn controls each cell in the body. This includes how quickly the cell grows, how often it divides, and how long it lives. Mutations happen often and can be beneficial, harmful, or neutral, depending on where the change occurs. Gene mutations happen when we are exposed to something around us that damages our genes, like cigarette smoke. The body can self-correct most mutations without any consequences. Gene mutations can also be inherited from a parent.
It’s important to realize that not all mutations cause cancer but all cancers begin when a combination of mutations cause cells to multiply uncontrollably.1 Over a lifetime, mutations can build up. Cancer more frequently occurs from multiple mutations—this is why cancer occurs more often in the elderly.
Two Types of Genetic Mutations
- Acquired mutations. These are the most common cause of different cancers. They occur during a person’s lifetime and are not passed from parent to child. They are often influenced by environmental factors, such as tobacco use, UV radiation, viruses, and age.
- Germline mutations. These aren’t as common and happen at the time of conception. A mutation is present in a parent’s sperm or egg cell and is then copied into every cell within the fetus’ body. Up to 10% of all cancers may be caused by inherited genetic changes.2
Screening Recommendations for Cancer-Causing Mutations
Knowing you have a mutation creates the opportunity to decrease the risk through early cancer screenings and other measures.
Having a germline mutation, or an inherited genetic mutation that increases cancer risk, does not necessarily mean that a person is destined to get cancer. It does, however, mean that the risk is higher than average. Many people might ask themselves why anyone would want to know this worry-inducing information to begin with.
As researchers gain more understanding into genetic mutations, they’ve identified some of those that increase risk for breast cancers in both women and men, as well as colorectal, endometrial, ovarian, gastric, skin, pancreatic, and prostate cancers.3
Patients who have a known cancer-causing genetic mutation are considered “high risk” and often begin cancer screening tests earlier in life or have them done more frequently. In some cases, more robust testing is used than the standard regimen.
As always, consult your physician to discuss your individual risk factors and screening recommendations. The following are some examples of recommended screening regimens:
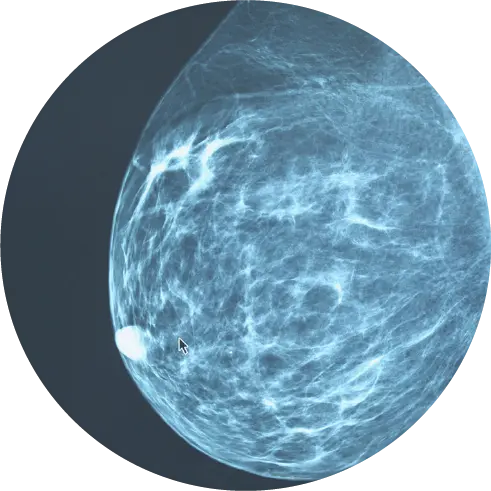
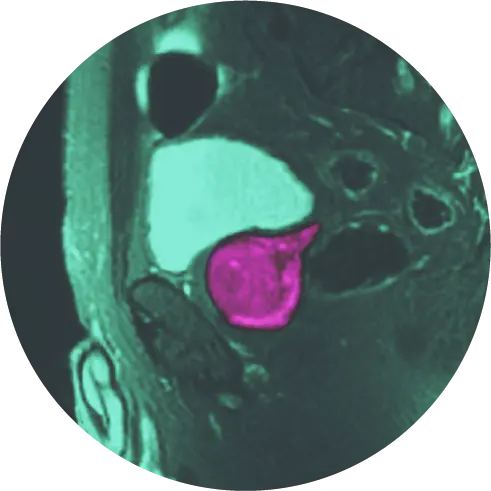
Breast Cancer
Patients who are at high risk for breast cancer should learn to do breast self-exams and do them monthly, beginning in the teenage years. This is the best way for women (and men) to familiarize themselves with how their breast tissue normally looks and feels, so that any early changes can be detected.
Additionally, according to the American Cancer Society, women who are high risk should get a breast MRI and a mammogram every year, typically starting at age 30.4
Gynecological Cancers
Cervical, ovarian, uterine, vaginal, and vulvar cancers are common malignancies in women, with approximately 5-10% of cases caused by genetic mutations. Some of the genes that cause these types of cancers are the same as for breast cancer. Women normally undergo cervical cancer screenings via Pap tests every 2-3 years, and HPV tests if unvaccinated.5 However, those at high risk may also need to do the following:
- Those at high risk for cervical cancer may need to get a Pap smear every year.
- To detect endometrial cancer, a transvaginal ultrasound and endometrial biopsy should be done every 2 years, beginning at age 30-35.
- Those at high risk for ovarian cancer can get CA-125 blood tests every year.
- Hysterectomy and bilateral salpingo-oophorectomy to prevent gynecologic cancers
Cervical, vaginal, and vulvar cancers are also caused by human papillomavirus (HPV), a very common sexually transmitted infection. It is recommended that everyone get this vaccine, starting at around age 11 to 12.
Colorectal Cancer
Like some other cancers, early-stage colorectal cancer has few symptoms. This makes early detection that much more important, as this is when treatments are most effective.
For those with genetic indicators for colorectal cancers, it is recommended to start getting colonoscopies every 1-2 years between the ages of 20-25 (or 2-5 years before the earliest colorectal cancer in the family).6
Prostate Cancer
Some of the same gene mutations that cause breast cancer and ovarian cancer, cause prostate cancer. If any of these cancers run in the family, individuals may have a higher risk for prostate cancer.
Men with genetic risk factors are recommended to start PSA testing at age 40 or at least 10 years prior to the youngest prostate cancer diagnosed in the family.7
Other Cancers
Other types of genetic mutations related to specific cancers have their own early screening recommendations, such as MRIs and ultrasounds. Genetic counseling and testing can assist you and your doctor determine the best screening regimen.
Who Should Get Genetic Testing?
Those who have a family history of cancer should consider genetic testing. Before engaging in genetic testing, even though it is readily available online, it is recommended that people first meet with a genetic counselor. Family physicians can easily make this referral. It is important for a specialist to examine the family history, order the right tests, and make sure the results are interpreted correctly. The goal of testing is not just to get a result, but to help guide and create a plan to reduce the risk of getting cancer.
Testing typically begins with the relative who was diagnosed with cancer. If there is no inherited mutation, then there is no reason for testing his or her children. Also, children should not be tested unless they are at an age when screenings should begin—for example, with mammography or colonoscopy. To find the appropriate guidelines to what ages screening should begin for certain cancers, please visit NCCN.org.
With the advent of genetic testing for cancer comes some worries when it comes to legal protections. For example, can insurance companies raise rates for someone with an increased breast cancer risk? The answer is NO. As a result of the Genetic Information Nondiscrimination Act of 2008 (GINA) and the Privacy Rule of the Health Information Portability and Accountability Act of 1996 (HIPAA), insurance providers, employers, or others cannot access this private information.8 Also, as a result of the Affordable Care Act, coverage cannot be denied because of a pre-existing condition or any certain health status.
References
1 American Society of Clinical Oncology. The Genetics of Cancer. Mar 2018. Retrieved Nov 3, 2022 from https://www.cancer.net/navigating-cancer-care/cancer-basics/genetics/genetics-cancer
2 National Cancer Institute. The Genetics of Cancer. Aug 17, 2022. Retrieved Nov 3, 2022 from https://www.cancer.gov/about-cancer/causes-prevention/genetics
3 Facing Hereditary Cancer Empowered. Table of different genes and the hereditary cancers that they cause. Feb 8, 2022. Retrieved Nov 3, 2022 from https://www.facingourrisk.org/info/hereditary-cancer-and-genetic-testing/genes-by-cancer-types
4 ACS Breast Cancer Screening Guidelines. (2022). Retrieved 8 November 2022 from https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html
5 Centers for Disease Control and Prevention. (2022). Cervical Cancer: What Should I Know About Screening? Retrieved Nov 8, 2011 from https://www.cdc.gov/cancer/cervical/basic_info/screening.htm
6 Centers for Disease Control and Prevention (2022). Hereditary Colorectal (Colon) Cancer: Medical Options. Retrieved 8 November 2022 from https://www.cdc.gov/genomics/disease/colorectal_cancer/medical_options.htm
7 Experts create guidelines for screening prostate cancer patients for inherited cancer risk genes. (2022). Retrieved 8 November 2022 from https://www.pcf.org/news/genetic-screening-guidelines-for-prostate-cancer
8 National Human Genome Research Institute. Timeline of the Genetic Information Nondiscrimination Act (GINA). Sept 16, 2020. Retrieved Nov 3, 2022 from https://www.genome.gov/about-genomics/policy-issues/timeline-genetic-information-nondiscrimination-act-GINA