As researchers find out more about what causes various cancers, it is apparent that many cases each year can be linked to lifestyle factors.
When it comes to cancer risk, there are two types of risk factors—modifiable and non-modifiable. Modifiable risk factors are, to some extent, within our control to change. Non-modifiable risks include genetic mutations, race, and age.
An important study published in the November 2017 issue of the American Cancer Society’s publication CA: A Cancer Journal for Clinicians analyzed the number of cancer cases that could be attributed to lifestyle factors and the proportion that could have possibly been prevented. This comprehensive study looked at a broad range of lifestyle factors and 26 different cancer types in adults ages 30 years and older. The meta-analysis concluded that an estimated 42% of all incident cancers (659,640 of 1,670,975) and 45.1% of cancer deaths (265,150 of 587,521) were attributed to modifiable risk factors.1
What Are the Lifestyle Risk Factors?
A lot of data goes into determining correlations between lifestyle factors and the cancer types they are associated with. Many times, these lifestyle factors are familial or related to childhood living conditions. These lifestyle factors are complicated and can be difficult to resolve. The following chart lists the risk factors and their corresponding associated cancers from the American Cancer Society.
Figure 1. Risk Factors Associated with Increased Cancer Risk
| RISK FACTOR | CANCER TYPE |
| Smoking | Oral cavity, pharynx, esophagus, stomach, colorectum, liver, pancreas, nasal cavity/paranasal sinus, larynx, lung, bronchus, trachea, cervix, kidney, renal pelvis, ureter, urinary bladder, acute myeloid leukemia |
| Exposure to secondhand smoke | Lung, bronchus, trachea |
| Excess body weight | Esophagus, stomach, colorectum, liver, gallbladder, pancreas, female breast, corpus uteri, ovary, kidney, renal pelvis, thyroid, multiple myeloma |
| Alcohol intake | Lip, oral cavity, pharynx, esophagus, colorectum, liver, larynx, female breast |
| Poor diet: Red meat consumption | Colorectum |
| Poor diet: Processed meats | Colorectum, stomach |
| Poor diet: Low fruit/vegetable consumption | Oral cavity, pharynx, larynx, lung, bronchus, trachea |
| Poor diet: Low dietary fiber consumption | Colorectum |
| Poor diet: Low dietary calcium consumption | Colorectum |
| Physical inactivity | Colon, excluding rectum, female breast, premenopausal and postmenopausal cancers, corpus uteri |
| Ultraviolet radiation | Melanoma of the skin |
| Infection: Helicobacter pylori | Stomach |
| Infection: Hepatitis B | Liver |
| Infection: Hepatitis C | Liver, non-Hodgkin lymphoma |
| Infection: Human herpes virus type 8—Kaposi sarcoma herpes virus | Kaposi sarcoma |
| Infection: Human immunodeficiency virus (HIV) | Anus, Kaposi sarcoma, cervix, Hodgkin lymphoma, non-Hodgkin lymphoma |
| Human papillomavirus (HPV) | Oral cavity, oropharynx, tonsils and base of tongue, anus, cervix, vulva, vagina, penis |
Some of these factors and their associated cancers are controllable by individuals and their families. Some factors, like secondhand smoking, are more difficult to control and mitigate.
How Can I Reduce My Risk?
Stop smoking—or don’t start.
In the above cited study, cigarette smoking accounted for the highest proportion of cancer cases and deaths, above all the other risk factors. If people do ONE thing to reduce their cancer risk, stopping smoking would be the most impactful. 1
Each cigarette puff issues a mixture of chemicals straight to the lungs, where they are absorbed quickly into the bloodstream. From there, these chemicals are carried to every organ in the body. This is one reason that smoking has the potential to cause a wide range of cancer types in many organs. These damaging chemicals damage cell DNA—which can cause cells to mutate and grow uncontrollably—starting down the path to cancer. Tobacco smoke contains more than 7,000 chemicals—at least 70 of which are known to cause cancer.2
Cigarettes are very addictive and difficult to quit. Most people do not quit on their first attempt. However, there are many resources out there to help. Many find that it takes a combination of methods for them to permanently kick the habit.
What about vaping? While vaping doesn’t have the long-term depth of research that cigarette smoking does, there is some existing evidence that vaping increases the risk for cancer. One of the difficulties in studying the direct links to vaping and cancer is the wide variety of e-fluids available and their differences in chemical makeup. It can also take decades before the long-term effects of vaping can appear. Most vape users are under the age of 35. Most people who vape have also been cigarette smokers at some point. In fact, only 15% of people who vape have never smoked. More research is needed to conclusively determine the link between vaping and cancer, but most physicians recommend against it.3
Limit exposure to secondhand smoke.
Whether you are living with a smoker or are the one potentially exposing others to the effects, you need to know that secondhand smoke can be deadly. Secondhand smoke exposure includes two types: side stream smoke (smoke from the burning tip of the cigarette) and mainstream smoke (smoke exhaled by a smoker).
Public opportunities for secondhand exposure have been mitigated over the years as smoking indoors has become a rarity. Workplaces, bars, restaurants, and recreational settings in most areas have gotten rid of their smoking sections. However, the home is a primary source of exposure for infants, children, and non-smoking adults. Vehicles come in a close second.
Many of the chemicals that are inhaled by smokers are also present in secondhand smoke, including those that cause cancer.
Steps you can take to take to protect yourself and your family:4
- Do not allow smoking in your home.
- Do not allow smoking in your car, even with windows down.
- Make sure places where children are cared for are free of secondhand smoke.
- Teach children about secondhand smoke and avoiding it.
- Frequent restaurants and bars that are smoke-free.
- Protect your family by being a good role model and not smoking.
Maintain a healthy body weight.
Most people know that being overweight or obese carries health risks, such as heart disease, diabetes, stroke, and mobility issues. However, excess body weight carries a high risk for developing several types of cancer—second to only cigarette smoking. Excess body weight is thought to contribute to one in five cancer-related deaths in the U.S.5 Over 42% of adults in the U.S. are considered obese, with a BMI over 30, and the incidence of childhood obesity is on the rise. This unfortunate trend does not bode well for cancer rates in upcoming years.
Excess body fat causes hormone levels in the body to change, many of which can cause mutations in genes. For example, overweight women typically have higher estrogen levels, and men have lower testosterone levels. Obesity can also cause inflammation and higher than normal levels of insulin and growth factors, which also increases risk.
What can you do to lower your risk? Lifestyle modifications like eating a balanced diet that is low in refined sugars, hydrogenated fats, and fast foods can reduce hunger and insulin spikes. Getting regular physical activity helps burn calories and build muscle that raises metabolism. Even a moderate weight loss can significantly reduce inflammation and hormone abnormalities that increase cancer risks.
Make healthy food choices, avoid excess alcohol.
The American Cancer Society recommends the following:6
- Eat a diet rich in fruits, vegetables, and whole grains. Consume at least 2.5 cups of fruits and vegetables each day.
- Limit the intake of soy. High soy intake has been associated with hormone-sensitive cancers in women.
- Limit the intake of red and processed meats. Processed meats often contain nitrates and nitrites as preservatives, which are associated with increased risk for colorectal cancer.7
- Avoid excess alcohol consumption (no more than two drinks per day for men and one per day for women).
- Eat more omega-3 fatty acids, such as fatty fish, flaxseed oil, and walnuts.
- Eat less omega-6 fatty acids, such as corn oil, safflower oil, and sunflower oil.
- Avoid sugary drinks.
Reduce sun exposure and use daily sunscreen.
Ultraviolet (UV) radiation comes from the sun, sunlamps, and tanning booths, which can cause early aging of the skin and damage that can later lead to skin cancer. Peak sun exposure times are between mid-morning and late afternoon. People should try to avoid excessive exposure during these times and wear protective hats and clothing, as well as a good sunscreen.
Sunscreen products should contain at least SPF 15 and be applied about 30 minutes before going outside. It is also important to remember to re-apply at least every two hours, more often if in the water.
Use safe sex practices.
Sexually transmitted infections, some of which can have no symptoms, are major risk factors for developing cancer. Human papillomavirus (HPV) is a sexually transmitted virus, the same one that is responsible for genital warts. There are over 100 different types of HPV, some of which are strongly associated with cervical cancer. Approximately two-thirds of all cervical cancers are caused by HPV types 16 and 18, which are some of the most common types. A vaccine is available that prevents these types of HPV and is offered beginning in the adolescent years to both females and males.
Unfortunately, HPV is very common—with at least 20 million Americans that already have it, and an estimated 6 million more that acquire it each year. The CDC estimates that more than half of all sexually active adults will contract HPV during their lifetime.8
HPV can be spread through vaginal, oral, and anal sex. Men can also have HPV and spread it to their partners. Condoms should be used to reduce the spread, and people with multiple sex partners should get tested frequently.
Besides HPV, HIV infection (the virus that causes AIDS) is associated with specific types of cancers. Safe sex practices are the best protection against contracting HIV.
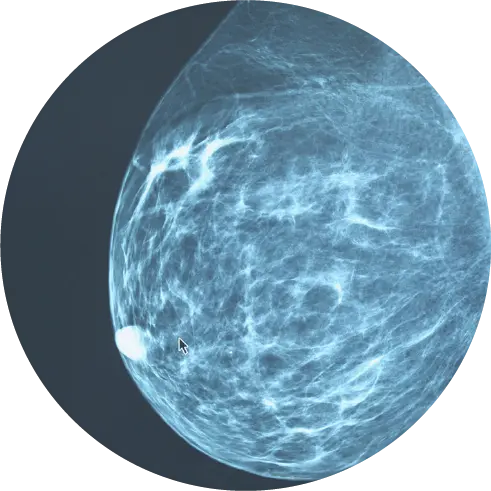
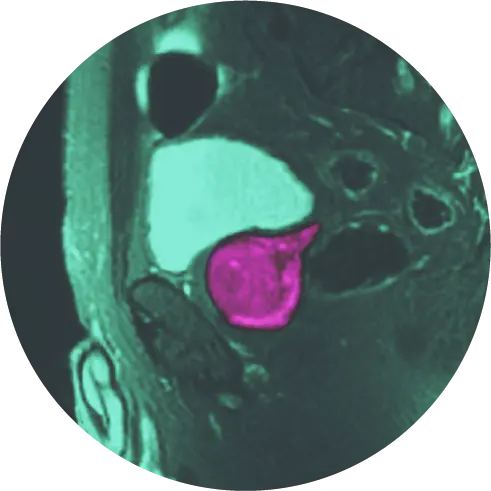
Get regular checkups and recommended cancer screenings.
It is important to maintain a regular schedule of cancer screenings for cervical, skin, breast, prostate, and colon cancers, according to your doctor’s recommendations. If you are at higher risk due to genetic or lifestyle factors, you may need additional tests such as MRIs, or more frequent screenings.
References
1 Islami, Farhad, MD, PhD; Goding, Ann Sauer, MSPH; Miller, Kimberly D. MPH et.al. (2017) Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA: Cancer J Clin 2018:68 pp 31-54.
2 Centers for Disease Control and Prevention. (2022). Smoking and Cancer. Surgeon General’s Report on Smoking and Health. Accessed 16 December 2022 from: https://www.cdc.gov/tobacco/data_statistics/sgr/50th-anniversary/pdfs/fs_smoking_cancer_508.pdf
3 Vandergriendt, Carly. (2019) Does Vaping Actually Cause Cancer? Retrieved 16 December 2022, from https://www.healthline.com/health/can-vaping-cause-cancer#overall-risk-for-cancer
4 National Cancer Institute. (2022). Secondhand Smoke and Cancer. Retrieved 16 December 2022, from https://www.cancer.gov/about-cancer/causes-prevention/risk/tobacco/second-hand-smoke-fact-sheet
5 National Cancer Institute. (2022) Weight | Cancer Trends Progress Report. (2022). Retrieved 16 December 2022, from https://progressreport.cancer.gov/prevention/weight
6 National Library of Medicine. (2022). Diet and cancer: MedlinePlus Medical Encyclopedia. Retrieved 16 December 2022, from https://medlineplus.gov/ency/article/002096.htm
7 Gunnars, Kris, BSc. Are Nitrates and Nitrites in Foods Harmful?. (2022). Retrieved 16 December 2022, from https://www.healthline.com/nutrition/are-nitrates-and-nitrites-harmful
8 Healthline. (2017). Cervical Cancer Causes: HPV, Sex, and Other Risks. Retrieved 16 December 2022, from https://www.healthline.com/health/cervical-cancer-causes