MR Guided Laser Focal Therapy for Benign Prostatic Hyperplasia (BPH) - Patient Informed Consent
Please watch this consent video carefully and completely in order to prepare yourself, family members, and caregivers for the procedure. Do not skip ahead. It is essential that you watch it in its entirety. We want you to be as prepared as possible. This video describes the possible risks connected with performing laser focal therapy for prostate cancer. Should you have any questions or concerns, we strongly encourage you to contact our office prior to your procedure so that we may clarify any pertinent issues. “An educated patient is the best patient.”
To contact the HALO Diagnostics office and procedure location by phone, call (760) 776-8989
We are here to support you, please contact us if you have any questions or need assistance of any kind.
Purpose
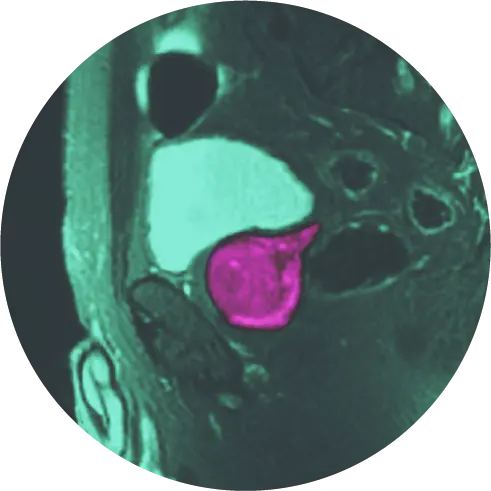
The purpose of this is to utilize MR (magnetic resonance) guided laser focal therapy for Benign Prostatic Hyperplasia (BPH). MR uses large magnets and radio waves to generate images of organs in the body. The laser uses light to heat a target area to destroy cancerous cells.
The laser system that will be used has been used for the treatment of brain, bone (spine), thyroid, and liver cancers.
The laser applicator placement will be performed using the Invivo DYNALOC software and DynaTRIM trans-rectal biopsy guidance system. This system is cleared (approved) by the U.S. Food and Drug Administration (FDA) for such uses.
Definition
Laser focal therapy of the prostate gland is a minimally invasive alternative to the standard treatment of Benign Prostatic Hyperplasia (BPH) and is considered experimental. It is a targeted procedure that focuses on a single area of the tumor as opposed to whole-gland therapy.
For the procedure, a laser applicator is introduced under MRI guidance via the rectum. Once in the gland, a nontherapeutic “test” dose is administered to verify proper placement in the target, then increased while “real-time” temperature change is displayed on a thermal map. Once the entire area is treated (approximately 2 minutes), the laser is turned off. The number of treatments depends on the size, number, location, and shape of the target lesion(s).
Preparation
The procedure cannot be done if you are currently on or have recently taken any anticoagulant medication that may interfere with your ability to clot your blood (“blood thinners”). We will have reviewed all of your current medications with you during the consultation, but please tell us if anything has changed since your previous visit. We need to make sure that your medication is not a blood thinner. The most common of these medications are aspirin and all related pain reliever or anti-inflammatory compounds (whether prescription or over-the-counter).
You will need to fast for 8 hours prior to prostate laser focal therapy. Do not eat any food or consume any liquids during this time period. We want to avoid gas or stool in the rectum. Upon arrival, you will be provided an enema. Depending on the treatment location, you may have a urinary catheter inserted prior to the procedure.
You may be given an oral antibiotic which should be taken as directed by our physicians. Most patients will simply receive intravenous antibiotics at the time of the procedure.
You must have a friend or family member come with you to your appointment to drive you home and remain with you overnight. This is extremely important since you will receive conscious sedation. Plan to remain in the area for at least two days after your procedure for observation. If you cannot bring a friend or family member there are local services that can provide you with overnight care the day of your procedure.
Procedures
Baseline Evaluation Procedures
Prior to laser focal therapy, the following study procedures will be performed.
- Medical history and quality-of-life questionnaires.
- Blood tests – including but not limited to PSA.
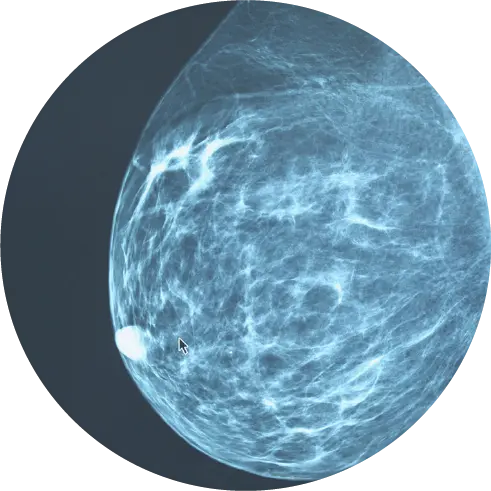
- Multiparametric MRI of the prostate – including MRI with contrast (gadolinium).
- Estimate of prostate gland volume.
Treatment Procedures
The actual procedure typically takes up to 4 hours. You will have a local anesthetic and be given an IV sedative medication before the procedure. You will also receive a regional anesthetic which is injected into both sides of the prostate gland. You will get a urinary catheter placed before your procedure if the tumor is down low in the apex, or afterward to preserve urine flow as the prostate can swell from inflammation. You’ll be placed lying face down on the MRI table. A laser guide will be gently placed in your rectum. Although it is slightly uncomfortable, very few patients believe it is painful. After confirming the precise position of the small laser applicator with MRI, we will then treat the target area(s). The amount of time the laser is on will depend on the decision of the surgeon, your anatomy, and possibly on whether you have had a therapy done in the past.
At the end of the laser treatment, post-treatment MR imaging will be performed.
Post Procedure
After the procedure, you might feel a bit sore in the rectal or anal area for a few hours. Patients with hemorrhoids might have discomfort a bit longer. It is very common to see some blood from the rectum, on the stool with the next bowel movement, or on the toilet paper especially that day and rarely the next day. Again, this is more common in patients with hemorrhoids. A small amount of blood in the urine or some discoloration of the urine is also a possibility. You may commonly see blood in your semen (ejaculation) for 1-2 days and sometimes up to 6 weeks. It might be red or just discolor your semen brown.
You are restricted from driving immediately following the treatment. You have no other restrictions after the procedure other than to take it easy that day and not engage in strenuous activity for 4-6 weeks. Have a family member or friend drive you home following the procedure.
At the discretion of your radiologist/interventional radiologist/surgeon, you may go home with a urinary catheter in place. This is temporary and the duration will depend on the size and location of the treatment(s).
Post-treatment Evaluation
Two days post-treatment you will receive a pelvic ultrasound to evaluate your bladder
Possible Complications of the Procedure
This procedure, regardless of complexity or time, may be associated with unforeseen problems. Problems may be immediate or even quite delayed in presentation. While we have discussed these and possibly others in your consultation, we would like you to have a list so that you may ask questions if you are still concerned. Aside from anesthesia complications, it is important that every patient be made aware of all possible outcomes which may include, but are not limited to:
- Pain and/or discomfort
- Excessive Bleeding from the Rectum/Anus: It is uncommon to require any treatment and the majority of the time bleeding stops on its own. This is far more common in patients with hemorrhoids or arterial bleeding. In the unusual circumstance that excessive bleeding occurs or a severe infection occurs this may require emergency room care and possible hospitalization.
- Blood Clots in the Urine: The device can enter the middle of the prostate where the urethra or the neck of the bladder are located and cause blood in the urine. If the bleeding is significant, it can cause clots that can block the urine flow. A urinary catheter will be inserted to avoid this problem. It has been our experience that while the catheter might be uncomfortable it helps to avoid possible issues.
- Urinary Retention: Even in the absence of bleeding, the prostate can become swollen from the treatment or secondary to infection.
This is another reason why post-procedure urinary catheter placement is important. Usually, the problem resolves with time after the swelling goes down. Patients at greater risk are those who already have difficulty urinating before the procedure due to BPH (Benign Prostatic Hyperplasia).
- Urinary Tract Infection or Urosepsis: Although you will receive IV antibiotics, it is possible for you to get an infection. It might be a simple bladder infection that presents with symptoms of burning urination, urinary frequency, and a strong urge to urinate. This will usually resolve in a few days with antibiotics. If the infection enters the bloodstream, you may feel very ill. This type of infection often presents with urinary symptoms and any combination of the following: fevers, shaking, chills, weakness or dizziness, nausea, and vomiting. You may need a short hospitalization for intravenous antibiotics, fluids, and observation. This is more common in diabetics, patients on long-term steroids, or patients with any disorder of the immune system. Lastly, an abscess of the prostate, while quite rare, can develop. This is an infection cavity that may respond to antibiotics alone or need surgical (needle) drainage. It can begin with urinary symptoms but also progress to the symptoms of bloodstream infection. Urinary retention is also possible with an abscess.
- Erectile Dysfunction (ED): Inability to achieve or maintain an erection can occur following this procedure in less than 1% of patients. This condition may be temporary or permanent. A decrease in the volume of seminal fluid is also a possibility. This may result in infertility.
- Urinary Incontinence: The ability to voluntarily control urination may be lost in less than 1% of men undergoing this procedure. This may be a temporary or permanent condition.
- Tingling/Numbness of the Penis or Scrotal Pain: Some men may feel an urge to urinate during the procedure. Some feel tingling in their penis or scrotum due to referred pain. Similar to when you hit your funny bone, your fingers may tingle. These sensations generally stop after each 2-minute treatment, and rarely persist after the procedure. This condition usually resolves over weeks to months. Scrotal pain has also been reported following the procedure.
- Rectal Fistula: Rarely an abnormal connection between the rectum and the urethra or urinary bladder may develop. This may require surgery for treatment. Our team devised a method to place safety boundaries over important structures like the rectal wall to avoid this serious problem.
- Thermal injury to nearby organs: Injuries due to the heat produced by the laser have not been seen in patients to date; however, there is a possibility that heat damage could occur if the laser fiber has a crack along its length. We prevent this by visually inspecting every fiber prior to its use to ensure is being emitted only from the tip.
- Carbonization of laser applicator: This may result in a portion of the applicator being retained inside the prostate or being expelled.
- Possible need to have further procedures or TURP: this surgical procedure removes excess prostate tissue.
- Possible scar in the urethra (rare).
- Possible persistent obstructive or irritative urinary symptoms.
The gadolinium contrast agent used with MRIs has known risks. The most common are:
- strange tastes;
- changes in smells;
- injection site reactions;
- nausea;
- generalized feeling of warmth; headache; and
- dizziness.
Rarely, serious, life-threatening allergic-type reactions can occur.
If you have symptoms of any of the above, especially those of infection, you must contact the office of Dr. John F. Feller immediately or go to the nearest Urgent Care or emergency room.
Alternatives
Your alternatives to this procedure include:
- active surveillance
- radical prostatectomy
- radiation therapy
- brachytherapy
- androgen deprivation therapy
- another experimental treatment/procedure
The doctor will discuss these alternatives with you.
Confidentiality
Your information may also be given to the U.S. Food and Drug Administration (FDA). It may be given to similar governmental agencies in other countries. Medical records which identify you and the consent form signed by you may also be looked at and/or copied for research or regulatory purposes by:
- Department of Health and Human Services (DHHS) agencies,
- the institution where the research is being done,
- the California Cancer Registry, and
- Western Institutional Review Board® (WIRB®).
Although absolute confidentiality cannot be guaranteed because of the need to give information that identifies you to these parties, we make every effort to anonymize information for all of our patients.
Whom to Contact
For answers to questions relating to this procedure, or to report a concern, complaint, or research-related injury, or for information regarding laser procedures you may contact:
HALO Diagnostics: 760-776-8989
Bernadette M. Greenwood
760-776-8989 x747 (24 hours)
262-269-8764 (24 hours)
If you are experiencing any medical emergency, dial 9-1-1 or go to the emergency room or urgent care.
By signing the physical Informed Consent Document, you will be agreeing to undergo magnetic resonance image-guided transrectally delivered laser-induced interstitial thermal therapy for laser focal therapy of Benign Prostatic Hyperplasia in an outpatient setting.